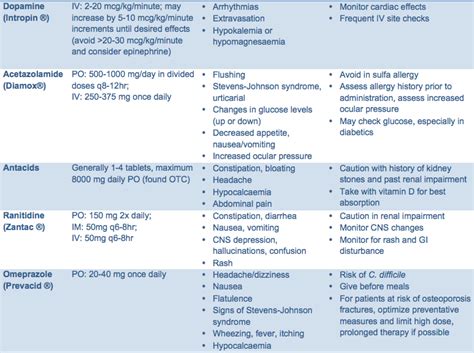
Causes Of Pancreatitis Medications

Understanding the Link Between Medications and Pancreatitis
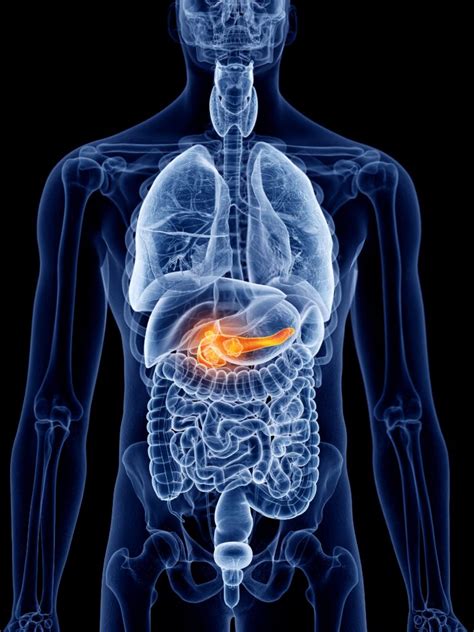
Pancreatitis, an inflammation of the pancreas, can be a painful and potentially serious condition. While the exact causes are not always clear, certain medications have been identified as potential triggers. It's important to recognize the role these medications play in pancreatitis development to ensure proper management and prevention.
Medications Linked to Pancreatitis

Numerous medications have been associated with pancreatitis, with varying levels of evidence. Here are some of the key categories and specific drugs that have been implicated:
Antiviral Medications
- Aciclovir: Used to treat viral infections like herpes and chickenpox, aciclovir has been linked to pancreatitis, especially in children and those with pre-existing kidney problems.
- Valacyclovir: A prodrug of aciclovir, valacyclovir has also been associated with pancreatitis, although the risk is considered low.
Antiretroviral Drugs
- Didanosine: Commonly used to treat HIV/AIDS, didanosine can cause pancreatitis, particularly in children and those with a history of pancreatitis.
- Zidovudine: Another antiretroviral drug, zidovudine has been linked to pancreatitis, especially when used in combination with other drugs like didanosine.
Antibiotics

- Pentamidine: An antibiotic used to treat infections like pneumonia and leishmaniasis, pentamidine can cause pancreatitis, especially when administered intravenously.
- Azathioprine: An immunosuppressant drug often used to prevent organ rejection, azathioprine has been associated with pancreatitis, particularly in patients with a history of the condition.
Anticoagulants
- Warfarin: A commonly used anticoagulant, warfarin has been linked to pancreatitis, especially in patients with a history of the condition or those taking high doses.
Chemotherapy Drugs
- Gemcitabine: Used to treat various cancers, gemcitabine has been associated with pancreatitis, especially in patients with a history of the condition or those taking high doses.
- 5-Fluorouracil: Another chemotherapy drug, 5-fluorouracil has been linked to pancreatitis, particularly when used in combination with other drugs.
Other Drugs

- Furosemide: A diuretic used to treat fluid retention, furosemide has been associated with pancreatitis, especially in patients with pre-existing kidney problems.
- Sulfa Drugs: Sulfonamides, commonly used as antibiotics, have been linked to pancreatitis, particularly in patients with a history of the condition or those taking high doses.
How Medications Cause Pancreatitis
The exact mechanisms by which medications cause pancreatitis are not fully understood. However, several theories exist:
- Direct Toxicity: Some medications may directly damage the pancreas, leading to inflammation.
- Drug Interactions: Certain drug combinations can increase the risk of pancreatitis, possibly due to synergistic effects or increased toxicity.
- Immune-Mediated: In some cases, medications may trigger an immune response that leads to pancreatitis.
- Metabolic Disturbances: Certain drugs can disrupt normal metabolic processes, leading to the release of toxic substances that damage the pancreas.
Risk Factors and Prevention

While anyone taking these medications is at risk, certain factors can increase the likelihood of developing pancreatitis:
- Pre-existing Conditions: Patients with a history of pancreatitis, kidney problems, or metabolic disorders are at higher risk.
- Dosage and Duration: Higher doses and longer treatment durations may increase the risk of pancreatitis.
- Age and Genetics: Children and those with a family history of pancreatitis may be more susceptible.
To prevent medication-induced pancreatitis, it's crucial to:
- Follow prescribed dosages and treatment durations.
- Inform healthcare providers of any pre-existing conditions or allergies.
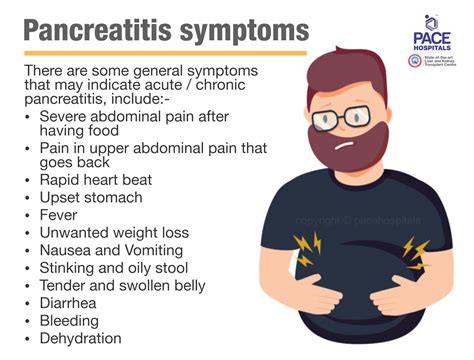
- Report any symptoms of pancreatitis, such as severe abdominal pain, nausea, or vomiting, to your healthcare provider immediately.
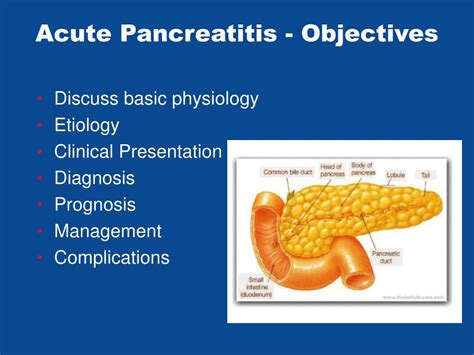
Diagnosis and Treatment

Diagnosing medication-induced pancreatitis involves a combination of medical history, physical examination, and laboratory tests. Imaging studies like CT scans or MRIs may also be used to assess the extent of inflammation.
Treatment typically involves stopping the suspected medication and managing the symptoms. This may include pain management, intravenous fluids, and nutritional support. In severe cases, hospitalization and intensive care may be required.
Conclusion

While medication-induced pancreatitis is a serious concern, it's important to remember that most medications are safe when used as directed. By understanding the potential risks and taking preventive measures, patients and healthcare providers can work together to minimize the chances of developing this condition. As always, open communication with healthcare professionals is key to ensuring safe and effective medication use.
Can any medication cause pancreatitis?

+
While many medications have been linked to pancreatitis, the risk varies widely. Some drugs have a very low risk, while others have a higher likelihood of causing the condition. It’s important to discuss any concerns with your healthcare provider.
What are the symptoms of medication-induced pancreatitis?

+
Symptoms may include severe abdominal pain, nausea, vomiting, fever, and a rapid pulse. If you experience these symptoms while taking medication, seek medical attention immediately.
How is medication-induced pancreatitis treated?
+
Treatment typically involves stopping the medication and managing the symptoms. This may include pain management, intravenous fluids, and nutritional support. In severe cases, hospitalization may be required.
Can I prevent medication-induced pancreatitis?
+
While it’s not always possible to prevent medication-induced pancreatitis, taking medications as directed, informing your healthcare provider of any concerns or pre-existing conditions, and being aware of potential side effects can help reduce the risk.
What should I do if I suspect medication-induced pancreatitis?
+If you experience symptoms of pancreatitis while taking medication, seek medical attention immediately. Do not stop taking the medication without consulting your healthcare provider first.